 According to the C.D.C., in 2015, more than 78 million U.S. adults were obese.
According to the C.D.C., in 2015, more than 78 million U.S. adults were obese.
In 1980, no state in the U.S. had an adult obesity rate above 15% (http://stateofobesity.org/obesity-rates-trends-overview/). In 1990, no state was above 20%. In 2000, no state was above 25%. In 2015, all states recorded obesity rates above 20%. 24 states currently have obesity rates above 25%, and 12 states currently have obesity rates of above 30%.
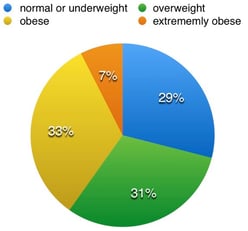
Nationwide today, roughly 31% of U.S. adults are overweight (BMI between 25 to 29.9) and 33% are obese (BMI ≥ 30) (https://www.niddk.nih.gov/health-information/health-statistics/Pages/overweight-obesity-statistics.aspx). Nearly 8% of adults are extremely obese with a BMI greater than or equal to 40. BMI, which is a measure of body fat based on your weight in relation to your height, is used to indicate ranges related to health risk: normal or underweight (BMI <24.9); overweight (BMI = 25 - 29.9); obese (BMI ≥ 30), extremely obese (BMI > 40).
The chart below shows the percentage of U.S. adults and corresponding BMI.
How does the obesity epidemic affect healthcare costs?
Obesity is one of the biggest drivers of healthcare costs in the U.S. Obesity-related health problems such as type 2 diabetes, hypertension and heart disease, joint problems, sleep apnea, and cancer represent an enormous cost to the healthcare system.
Currently, estimates for these costs range from $147 billion to nearly $210 billion per year. Obesity is associated with job absenteeism, costing approximately $4.3 billion annually and with lower productivity while at work, costing employers $506 per obese worker per year.
Reducing obesity, improving nutrition and increasing physical activity can help lower costs through fewer doctor's office visits, tests, prescription drugs, sick days, emergency room visits and admissions to the hospital and lower the risk for a wide range of diseases.
Primary Care and the Obesity Epidemic
With obesity statistics worsening year-over-year, it is clear that the United States has a weight problem.
Primary care practices, serving as the patients’ first point-of-contact with the health care system, are a crucial part of obesity management. However, screening and counseling for obesity is not occurring regularly during primary care visits. Nearly 50% of visits did not include a record of the height and weight data necessary to calculate BMI. 70% of clinically obese patients did not receive a diagnosis of obesity and 63% did not receive counseling from their physician. Thus, lack of provider documentation of obesity is linked to the absence of counseling patients about weight loss and the health risks of obesity.
While studies have shown that basic counseling about healthy behaviors takes less than five minutes, physicians often do not incorporate it into the visit.
Even for patients with documented obesity, physicians only discuss weight 65% of the time, recommend exercise 62% of the time, and refer patients for nutritional counseling 25% of the time. These low levels of counseling and referral indicate that there are barriers preventing physicians and patients from successfully initiating discussions about weight.
The dynamics of the physician-patient relationship also have a dramatic effect on the likelihood and success of counseling for weight loss during a physician visit. A 15-minute office visit hardly leaves enough time for the range of medical issues with which patients present.
Furthermore, physicians rarely have the training to effectively manage obese patients, given the underlying diet, exercise, cultural, and psychological issues that often need to be addressed to make significant headway. The patient-physician relationship is crucial to the physician’s ability to motivate the patient for weight loss and behavioral change, making the issue of stigma very important for discussions about improving primary care.
Physicians are being called on to adapt their practices to confront this obesity epidemic
As the prevalence and costs of health conditions associated with excess weight continue to rise, recognition and treatment of obesity as a medical condition is essential.
Increasing integration and care coordination is particularly important for obese patients. Monitoring weight and health risks would generate a consistent, long-term picture of the patient’s health status and improve the chances of early intervention.
Access to affordable, quality healthcare is important for maintaining good health. Doctors and other healthcare providers can provide guidance around nutrition and physical activity for patients, screen patients who are at risk for or who have developed obesity or obesity-related illnesses and provide counseling and support for ongoing care.
New models are also emerging to encourage and incentivize increased connection between doctor's care and support and services for people's daily lives. A number of healthcare providers and hospital systems have developed programs and policies to help support healthy nutrition and physical activity inside and beyond the doctor's office.
What's most important is extending the duration of primary care visits to sufficiently educate overweight and obese patients about the seriousness of their condition. But, as the demand for primary care doctors continues to outpace supply, it is only going to become more difficult for patients to schedule appointments with their doctors. Even if patients do schedule appointments, primary care doctor schedules are too overbooked, leading to shortened appointments. So, primary care doctors simply do not have the time to discuss all of the health issues related to obesity.
However, there is a solution that allows for patients to spend more time with their doctor to discuss health related issues along with treatments. The solution lies within enhanced personalized care granted through direct primary care.
Direct primary care offers the solutions to healthcare problems. Once enrolled with a direct primary care practice, patients have 24 / 7 access to their primary care doctor's cell phone along with the ease and convenience of scheduling same-day appointments. Many direct primary care practices don't have waiting rooms because there is no wait. Patients call in to schedule an appointment and they're in the doctor's office within a couple of hours. Can direct primary care help fix the obesity crisis in the United States?
If you or someone you know wants to lose weight and live a healthier, fuller life than consider direct primary care. The doctors at Total Access Medical are offering to meet with you for free. Find out how we can help you today.

