 Gowing older is an inevitable part of life. The older we get, the more common it is to experience mild soreness or aching when you stand, climb stairs, or exercise. But what does this mean for our joints and cartilage?
Gowing older is an inevitable part of life. The older we get, the more common it is to experience mild soreness or aching when you stand, climb stairs, or exercise. But what does this mean for our joints and cartilage?
Cartilage, which is the smooth, rubbery connective tissue on the end of bones, cushions joints and helps them move smoothly and easily. A lifetime of walking, exercising, and moving takes a toll on your cartilage and can cause degeneration, which causes chronic inflammation in the joint. This inflammation can further break down the cartilage and it may wear away completely if left untreated.
Osteoarthritis, also known as degenerative arthritis, degenerative joint disease, OA, or osteoarthrosis, is a form of arthritis caused by inflammation, breakdown, and the eventual loss of cartilage in the joints - the cartilage wears down over time. The joints most commonly affected by osteoarthritis are in the hands, feet, spine, and weight-bearing joints, such as the hips and knees.
In osteoarthritis, the top layer of cartilage breaks down and wears away. This allows bones under the cartilage to rub together. The rubbing causes pain, swelling, and loss of motion of the joint. Over time, the joint may lose its normal shape.
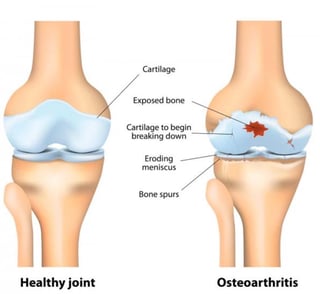
Also, bone spurs may grow on the edges of the joint. Bits of bone or cartilage can break off and float inside the joint space, which causes more pain and damage.
A common factor for developing osteoarthritis is age: most people with osteoarthritis are over the age of 55. Still, other factors increase a person’s chances for developing the disease. These factors include:
- Excess weight. Being obese or overweight puts additional stress on joints, cartilage, and bones, especially those in the knees. It also means you’re less likely to be physically active.
- Family history. Genetics may make a person more likely to develop osteoarthritis.
- Gender. Before age 45, men are more likely to develop osteoarthritis. After 50, women are more likely to develop osteoarthritis than men.
- Occupation. Certain occupations, such as those in construction, agriculture, cleaning, and retail, increase a person’s risk for developing osteoarthritis. Their bodies are used more rigorously as part of their job, which means their joints are worked more and likely age faster than people who have a desk job.
Younger, more active people can also develop osteoarthritis. However, it’s often the result of a trauma, such as a sport injury or accident. A history of physical injuries or accidents can increase a person’s chance of later developing osteoarthritis.
Treatments
Unfortunately, osteoarthritis is a progressive disease, which means signs and symptoms gradually worsen over time. There is no cure.
Instead, the goal of treatment is to manage pain, then reduce contributing causes that make the symptoms of osteoarthritis worse. The first step in treating osteoarthritis is to reduce pain. This is often initially done with a combination of medicines, exercise, and physical therapy.
Second, doctors will help patients adopt lifestyle changes that can prevent their individual osteoarthritis symptoms. Incorporating low-impact exercise and getting more rest can often extend the life of knees and joints without resorting to more invasive treatments.
Lifestyle and Alternative Treatments for Osteoarthritis
Having osteoarthritis does not mean you’ve reached the end of your physically active years. Instead, you will simply have to adjust the things you currently do to make them easier on your joints and bones. These adjustments not only improve function, but can also boost your quality of life.
- Exercise. Low-impact exercise can help strengthen muscles and keep bones strong. Exercise also improves joint mobility. Refrain from heavy-impact exercises, such as tennis and baseball, and begin doing more low-impact exercises such as golf, swimming, yoga, and cycling.
- Heat/cold therapy. Apply warm compresses or cold packs to joints when they are sore or painful. This can help relieve pain and reduce inflammation.
- Assistive devices. Using devices such as braces, splints, and canes can help your body support weak joints.
- Rest. Giving painful, sore joints adequate rest can relieve pain and reduce swelling.
- Weight loss. Losing as little as 5 pounds can help decrease the symptoms of osteoarthritis, especially in large joints, such as the hips and knees.

